Abbreviated DAPT strategy in an NSTE-ACS patient





Presentation, history and investigations
A 70-year-old man presented to our hospital in April 2023 with intermittent chest pain and shortness of breath of 7 days’ duration. He was a smoker with multiple comorbidities, including hypertension, diabetes mellitus (DM), hyperlipidaemia, ischaemic heart disease and history of peptic ulcer, for which he was receiving amlodipine 5 mg QD, metformin 500 mg BID, atorvastatin 40 mg QD, aspirin 80 mg QD, and pantoprazole 40 mg QD, respectively. He had a CT coronary angiogram in 2018 and it showed mild stenosis in the left anterior descending (LAD) artery, which was managed with aspirin 80 mg QD. The patient developed a haemorrhagic peptic ulcer associated with aspirin use in June 2021. After stabilizing the condition with pantoprazole and blood transfusion, a repeated oesophagogastroduodenoscopy (OGD) was performed, showing resolution of the ulcer. Aspirin treatment was continued along with pantoprazole.
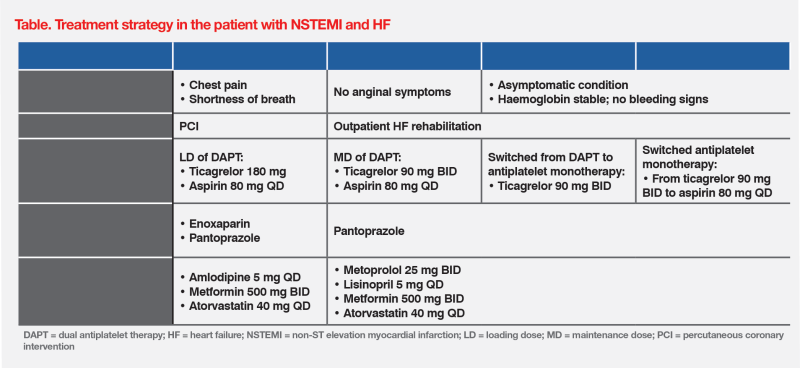
Upon admission, blood tests showed a markedly elevated level of cardiac Troponin I (5,000 ng/L), with an HbA1c level of 7.0 percent, an LDL-cholesterol level of 1.4 mmol/L, and haemoglobin 14.0 g/dL. Electrocardiography revealed ST depression in the LAD region, while echocardiography detected hypokinesia in the corresponding region and a left ventricular ejection fraction of 40 percent. The patient had no signs of anaemia. He was diagnosed with non-ST elevation myocardial infarction (NSTEMI) and heart failure (HF). (Table)
Management
The patient was started on a loading dose (LD) of dual antiplatelet therapy (DAPT) with ticagrelor (180 mg) and aspirin (80 mg).1 He was also given enoxaparin for acute coronary syndromes (ACS) and oral pantoprazole was continued for prevention of upper gastrointestinal (GI) bleeding. (Table)
Coronary angiography detected a lesion in the LAD artery, and percutaneous coronary intervention (PCI) was performed with implantation of a stent suited for short DAPT duration. After PCI, the patient experienced relief from anginal symptoms. He was prescribed a maintenance dose (MD) of DAPT with ticagrelor 90 mg BID and aspirin 80 mg QD, along with pantoprazole. He also continued treatments for DM and hyperlipidaemia. Because of his HF, amlodipine 5 mg QD was substituted with metoprolol 25 mg BID and lisinopril 5 mg QD.2 After 1 week of hospitalization, the patient was discharged and enrolled in outpatient HF rehabilitation. (Table)
While his condition remained stable on the DAPT regimen with ticagrelor and aspirin, the patient expressed concerns about the potential risk of gastrointestinal bleeding due to his medical history. His HAS-BLED score was 4 given his hypertension, history of bleeding, age of >65 years, and concomitant use of antiplatelet therapy. After thorough review and comprehensive discussion, he agreed to an abbreviated DAPT strategy involving 3-month DAPT followed by ticagrelor monotherapy (90 mg BID) for 9 months.1 (Table)
The patient remained stable and asymptomatic, with no chest pain while on ticagrelor-based abbreviated DAPT during the first 12 months after NSTEMI. He resumed daily activities and was able to enjoy time spent with his grandchildren. Notably, he did not experience any bleeding episodes. Upon completion of the abbreviated DAPT strategy, he was switched from ticagrelor to aspirin 80 mg QD monotherapy.1 As of April 2024, the patient remained on aspirin monotherapy for secondary prevention.1 (Table)
Discussion
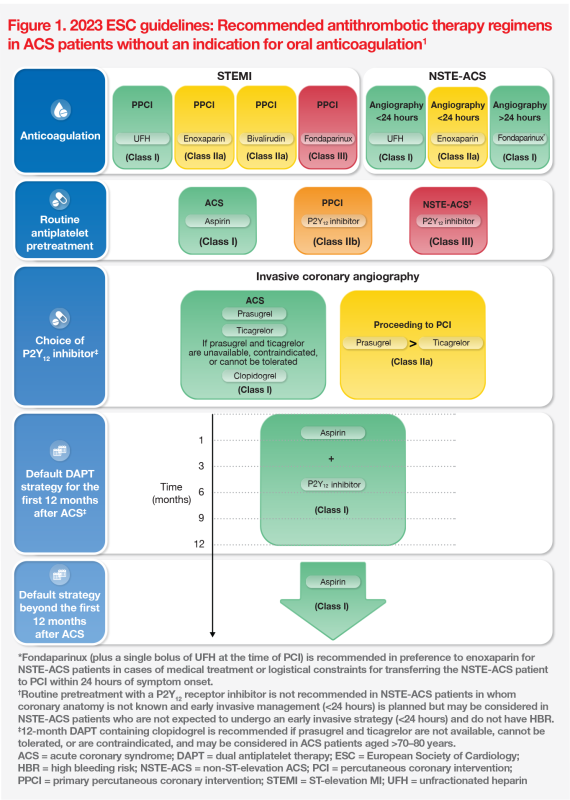
2023 guidelines of the European Society of Cardiology (ESC) for management of ACS (ie, non-ST elevation [NSTE]-ACS, ST-elevation MI [STEMI], unstable angina) recommend a DAPT regimen with a P2Y12 receptor inhibitor and aspirin (an initial oral LD followed by an MD for 12 months) for all patients, except those at high bleeding risk (HBR; Class I, Level A). Ticagrelor (oral LD, 180 mg; MD, 90 mg BID) is a P2Y12 receptor inhibitor recommended in conservative and invasive treatment strategies (Class I, Level B).1 (Figure 1)
ESC’s recommendation of ticagrelor plus aspirin as a standard DAPT regimen for ACS patients is based on findings from the phase III, double-blind PLATO study.1,3 In the study, 18,624 ACS patients (age <75 years, 84.5 percent; male, 71.6 percent; NSTE-ASC, 42.7 percent; PCI, 64.3 percent; coronary artery bypass grafting [CABG], 10.2 percent) were randomized to receive ticagrelor (n=9,333; LD, 180 mg; MD, 90 mg BID) or clopidogrel (n=9,291; LD, 300–600 mg; MD, 75 mg QD) in combination with aspirin as part of their DAPT regimen. Over the initial 12 months after ACS, patients on ticagrelor showed a significantly reduced rate of the primary composite endpoint of death from vascular causes, MI, or stroke vs patients on clopidogrel (9.8 vs 11.7 percent; hazard ratio [HR], 0.84; 95 percent confidence interval [CI], 0.77–0.92; p<0.001). The two groups showed no significant differences in rates of major bleeding (study criteria, 11.6 vs 11.2 percent; p=0.43) and life-threatening or fatal bleeding (study criteria, 5.8 vs 5.8 percent; p=0.70), although the use of ticagrelor was associated with a higher rate of non-CABG major bleeding vs clopidogrel (study criteria, 4.5 vs 3.8 percent; p=0.03).3
A subgroup analysis of PLATO’s NSTE-ACS patients (n=11,080; age <75 years, 82 percent; male, 69 percent; PCI or CABG during first 10 days, 52 percent) demonstrated a significant reduction in the primary composite endpoint of incidence of cardiovascular death, MI (excluding silent) and stroke in the ticagrelor vs clopidogrel group (10.0 vs 12.3 percent; HR, 0.83; 95 percent CI, 0.74–0.93; p=0.0013). The two groups had comparable rates of major bleeding (study criteria, 13.4 vs 12.6 percent; p=0.26) and life-threatening or fatal bleeding (6.6 vs 6.5 percent; p=0.56), despite a higher rate of non-CABG major bleeding with ticagrelor vs clopidogrel (study criteria, 4.8 vs 3.8 percent; p=0.0139).4
More potent antiplatelet agents may be associated with increased bleeding risk.5 To retain antithrombotic efficacy while reducing bleeding risk, DAPT strategy can be shortened or modified during the first 12 months after ACS.1,5
According to the 2023 ESC guidelines, DAPT abbreviation and DAPT de-escalation strategies may serve as alternatives to standard 12-month DAPT in specific cases to reduce the risk of bleeding events. In the DAPT abbreviation strategy, P2Y12 inhibitor monotherapy or aspirin monotherapy may be considered after 1 month of DAPT among patients at HBR (Class IIb, Level B). For patients who remain free from ACS events after 3–6 months of DAPT and who are not at high ischaemic risk, antiplatelet monotherapy, preferably with a P2Y12 receptor inhibitor, should be considered (Class IIa, Level A). At 30 days after ACS, de-escalation of P2Y12 receptor inhibitor therapy may be considered (Class IIb, Level A).1 (Figure 2)
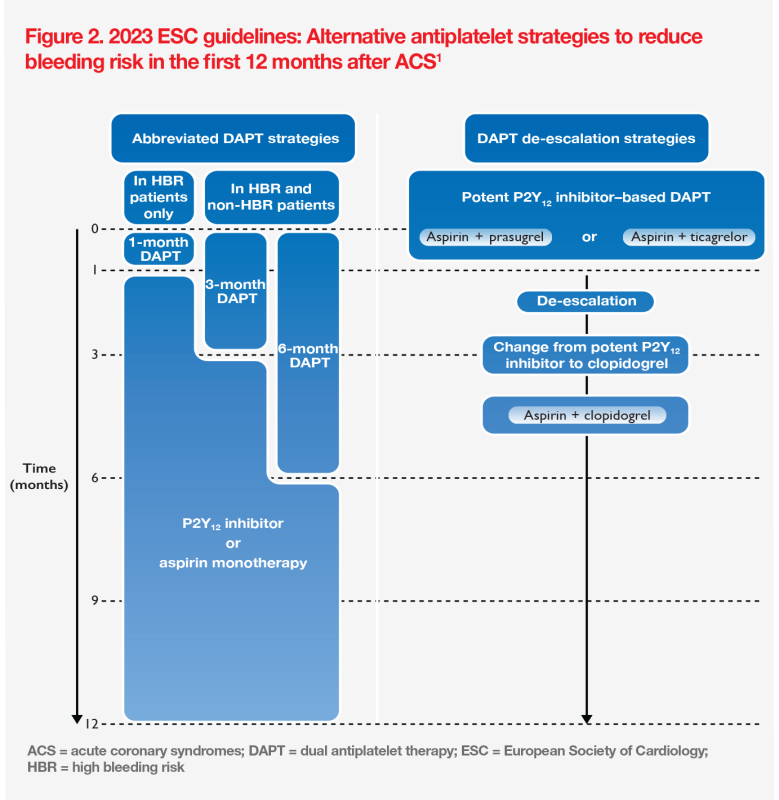
Our patient remained stable and free from anginal symptoms while on DAPT comprising ticagrelor and aspirin after PCI. However, he had a history of haemorrhagic peptic ulcer associated with aspirin, which necessitated OGD and blood transfusion. Consequently, he received 9 months of ticagrelor monotherapy following the initial 3-month DAPT regimen.1 With this abbreviated DAPT strategy, he remained well throughout the first 12 months after NSTEMI and did not experience any bleeding episodes.
From a cardiologist’s perspective, ESC’s 2023 guidelines for ACS management offer an effective and comprehensive algorithm with diverse antiplatelet strategies to address different scenarios of NSTE-ACS and STEMI cases. Importantly, the duration of DAPT should be tailored based on the individual patient’s clinical profile, with balance of ischaemic and bleeding risks and consideration of the type of stent implemented during PCI.1,6 ACS patients at HBR may require more frequent follow-up with haemoglobin monitoring. Self-monitoring for signs of bleeding, such as dark stools and epigastric pain, remains essential for timely intervention.
DAPT strategy optimization should be considered in ACS patients. Our case of an NSTE-ACS patient demonstrates the effectiveness of an abbreviated strategy with 3 months of ticagrelor-based DAPT followed by ticagrelor monotherapy in the first year post-ACS.