Addressing hyperphosphataemia with a polymer-based phosphate binder in a patient with ESRD




History and presentation
A 55-year-old male with end-stage renal disease (ESRD) started peritoneal dialysis (PD) in January 2020, with a regimen of nocturnal automated PD with 2 L of 1.5 percent dextrose six shifts per night and 2 L of 7.5 percent icodextrin during the day.
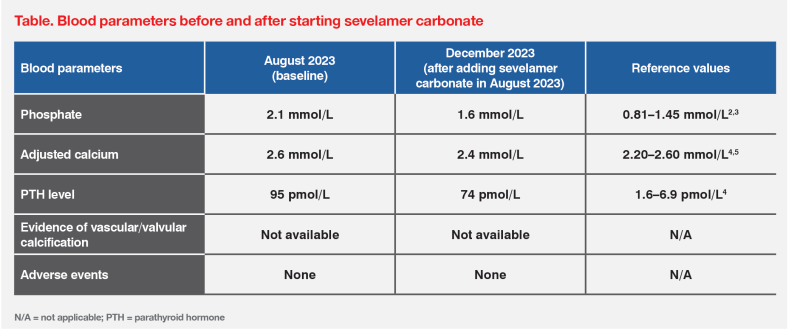
Alongside chronic kidney disease (CKD), he also had mineral bone disorder (CKD-MBD), and his baseline medications included calcium carbonate 3,000 mg TID and calcitriol 0.5 μg QD. In August 2023, the patient’s adjusted serum calcium level was 2.6 mmol/L, serum phosphate level was elevated at 2.1 mmol/L, alkaline phosphatase level was 82 IU/L, and parathyroid hormone (PTH) level was elevated at 95 pmol/L. (Table)
Treatment and response
Since the patient had a highnormal calcium level, hyperphosphataemia and hyperparathyroidism, his medications were adjusted. Calcium carbonate dose was reduced to 1,500 mg BID to lower the risk of complications associated with hypercalcaemia, and calcitriol dose was increased to 0.75 μg QD to help control his hyperparathyroidism. To address his hyperphosphataemia, the patient started treatment with sevelamer carbonate at 800 mg TID or 2.4 g/day taken over three meals per day, which is recommended for those with phosphate levels of 1.78–2.42 mmol/L.1 He was also referred to a dietician for low-phosphate diet awareness and education. Upon review, his dialysis regimen was found to be optimal.
Last seen in December 2023, the patient was assessed to be clinically well, with good adherence to his medication, diet and dialysis regimen. He was tolerating his treatments well, with no reported adverse effects (AEs). Follow-up laboratory results showed improvement in his CKD-MBD blood parameters, including adjusted calcium level of 2.4 mmol/L, phosphate level of 1.6 mmol/L, and PTH level of 74 pmol/L. (Table)
Since the patient is on dialysis, his serum calcium and phosphate levels will be monitored at least every 1–3 months and PTH levels every 3–6 months, based on recommendations for patients with severe CKD (ie, stage G5 or ESRD on dialysis) from the 2017 Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guidelines.6
Discussion
CKD-MBD is a systemic disorder characterized by a biochemical imbalance, specifically of calcium, phosphate, PTH and/or vitamin D levels, abnormalities in bone turnover and extraskeletal (eg, vascular, valvular) calcification, which are associated with increased risk of morbidity and mortality.7,8 Since these parameters are closely interrelated, the 2017 KDIGO Clinical Practice Guidelines recommend that treatments for patients with CKD-MBD should be based on combined serial assessments of serum phosphate, calcium, and PTH levels.6,7
In patients with CKD of any severity, excess and long-term calcium exposure through diet, medications or dialysate may be harmful due to the resulting hypercalcaemia and increased risk of vascular calcification. Higher calcium concentrations have been associated with increased risk of nonfatal cardiovascular (CV) events as well as increased mortality in adults.6
Similarly, elevated serum phosphate levels have been associated with increased vascular injury, including vascular and valvular calcification and atherosclerosis, as well as secondary hyperparathyroidism (SHPT), and concomitantly, poor prognosis.8-12
Hyperphosphataemia, in particular, is common in patients with CKD, affecting 50–74 percent of those with renal disorders.13,14 As kidney function progressively declines, mineral homeostasis becomes increasingly dysregulated and patients with ESRD on dialysis, such as our patient in this case, are likely to become hyperphosphataemic.15
For patients with hypercalcaemia and hyperphosphataemia, the KDIGO guidelines recommend lowering phosphate levels towards the normal range. In patients with moderate-tosevere CKD (ie, stage G3a–G5) who are already receiving phosphate lowering treatments, the dose of calcium-based phosphate binders should be restricted to avoid increasing calcium levels. Long-term use of aluminium-containing phosphate binders should also be avoided to prevent aluminium intoxication. Meanwhile, calcium-free phosphate binders may be considered due to the potential benefit, or at least absence of harm, vs calcium-based agents.6
In our patient’s case, the presence of a high-normal calcium level and hyperphosphataemia required dose reduction of calcium carbonate, consistent with the KDIGO recommendations. Since phosphate control is multifactorial, our patient was also encouraged to adhere to a lowphosphate diet. However, dietary intervention and a reduced calcium carbonate dose alone could not lower our patient’s phosphate level sufficiently due to his advanced CKD.6,12 Therefore, the calcium-free, polymer-based phosphate binder, sevelamer, was added to the patient’s regimen, as it provides phosphate-lowering efficacy without affecting serum calcium levels.1,6,16 It is also associated with a lower risk of coronary artery calcification, arterial stiffening and electrocardiogram abnormalities vs calcium-based phosphate binders.16,17
The 2-year, open-label, randomized INDEPENDENT (Reduce Cardiovascular Calcifications to Reduce QT Interval in Dialysis) study compared the effects of sevelamer vs calcium carbonate in 466 adult patients with stage G5 CKD (ie, patients who required dialysis <120 days). Results showed that patients who received sevelamer achieved significantly greater reductions in phosphate levels from baseline vs those who received calcium carbonate (-0.21 ± 0.04 mmol/L; p<0.001). Sevelamer was also associated with similarly significant reductions in calcium and PTH levels. Importantly, sevelamertreated patients had significantly lower CV mortality due to cardiac arrhythmias vs those who received calcium carbonate (hazard ratio, 0.06; 95 percent confidence interval, 0.01–0.25; p<0.001).16
Intake of phosphate binders is associated with increased pill burden.18 However, an open-label, randomized, cross-over study showed that 88 percent of patients were compliant with sevelamer treatment.19 Patients’ anticipated adherence to multiple pills should be considered when starting sevelamer therapy.
Restricting the dose of calcitriol or vitamin D analogues in case of persistent or recurrent hypercalcaemia is recommended in patients with moderate-to-severe CKD and hyperphosphataemia. 20 In our patient’s case, however, after lowering the dose of calcium carbonate and adding sevelamer, the dose of calcitriol was increased to control elevated PTH levels.
In summary, this case demonstrates that sevelamer carbonate, in combination with other phosphate binders and dietary control, offers an effective and well-tolerated treatment for hyperphosphataemia in patients with CKD-MBD, including those with advanced disease requiring dialysis.