First-line use of SGLT2 inhibitor as GDMT in a patient with HFpEF





History, presentation, and investigation
A 75-year-old female with a history of hypertension, diabetes, hyperlipidaemia, paroxysmal atrial fibrillation treated with apixaban (5 mg BID), and tachy-brady syndrome (for which a pacemaker was implanted in August 2022) was hospitalized due to acute shortness of breath (SoB) in November 2022.
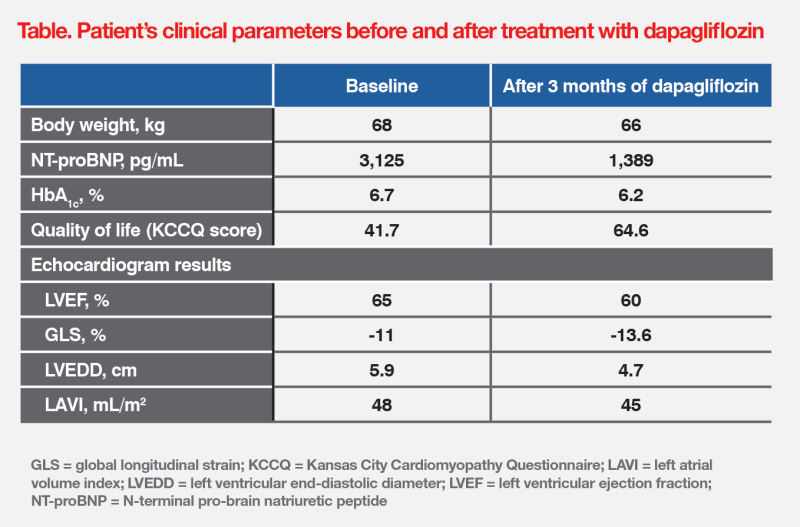
Chest X-ray indicated acute pulmonary oedema. Echocardiogram revealed left ventricular hypertrophy and severely dilated left atrium with a left ventricular ejection fraction (LVEF) of 65 percent. N-terminal pro-brain natriuretic peptide (NT-proBNP) level was elevated at 3,125 ng/mL. These findings were consistent with a diagnosis of heart failure with preserved ejection fraction (HFpEF). (Table)
Treatment and response
Upon admission, the patient was treated with continuous positive airway pressure (CPAP) ventilation and intravenous furosemide 20 mg, which led to successful decongestion. Spironolactone 12.5 mg QD was initiated 2 days before discharge.
The patient was discharged after 6 days of hospitalization. She received further management at our Ambulatory Heart Failure Clinic, where dapagliflozin 10 mg QD was initiated as part of guideline-directed medical therapy (GDMT). Furosemide was discontinued as the patient was clinically stable. Subsequently, metoprolol 75 mg BID was initiated and spironolactone was uptitrated to 25 mg QD.
Three months after starting dapagliflozin, the patient’s SoB and quality of life (QoL) improved, and her NT-proBNP level decreased to 1,389 pg/mL. Follow-up echocardiogram revealed improvements in left ventricular end-diastolic diameter (LVEDD), left atrial volume index (LAVI), and global longitudinal strain (GLS). (Table)
The patient tolerated dapagliflozin well without reporting any adverse events. During 18 months of follow-up, she remained well and stable, and did not require rehospitalization.
Discussion
Early diagnosis of HF is essential as it is associated with high mortality and rehospitalization rates.1-3 As shown in the above patient, diagnostic workup of suspected HF should include symptom assessment, electrocardiography, chest X-ray, NT-proBNP (if available), and echocardiography. NT-proBNP is a strong predictor of clinical outcomes and should be measured if the diagnosis is uncertain. HF is unlikely if NT-proBNP level is <125 pg/mL (<300 pg/mL for acute HF).4-5
According to the 2023 Focus Update of the European Society of Cardiology (ESC) HF Guidelines, HFpEF management involves:6
The prospective REDUCE-HF registry in Hong Kong adopted an intensive treatment strategy similar to that in the STRONG-HF trial in 245 patients discharged after hospitalization for acute HF. Results showed that rapid GDMT uptitration and close follow-up significantly lowered risks of all-cause mortality (2.5 vs 9.3 percent; hazard ratio [HR], 0.26; 95 percent confidence interval [CI], 0.18–0.41; p<0.001) and rehospitalization for HF (8.6 vs 13.1 percent; HR, 0.65; 95 percent CI, 0.55–0.74; p<0.01) at 90 days, and reduced NT-proBNP level by 45.2 percent (p<0.001), vs usual care.7
ESC’s recommendation of dapagliflozin as GDMT in HFpEF was based on the phase III, double-blind, randomized, controlled DELIVER trial, which evaluated dapagliflozin 10 mg QD vs placebo, added to usual therapy, in 6,263 patients with chronic HF and LVEF >40 percent. After a median follow-up of 2.3 years, dapagliflozin significantly reduced the risk of worsening HF or CV death (composite primary outcome; HR, 0.82; 95 percent CI, 0.73–0.92; p<0.001) vs placebo.6,8
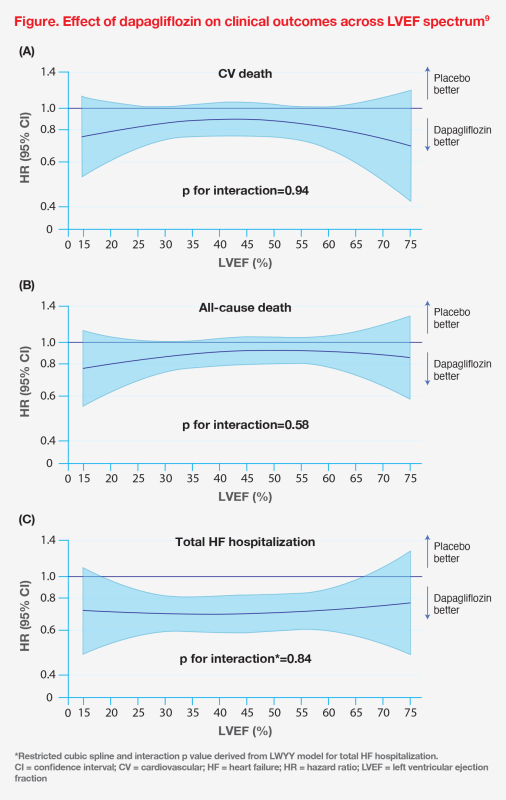
In a pooled meta-analysis of DAPA-HF and DELIVER in patients with HF and different ranges of LVEF (≤40 and >40 percent, respectively), dapagliflozin reduced risks of CV death (HR, 0.86; 95 percent CI, 0.76–0.97; p=0.01), all-cause death (HR, 0.90; 95 percent CI, 0.82–0.99; p=0.03) and total hospitalization for HF (rate ratio, 0.71; 95 percent CI, 0.65–0.78; p<0.001) in the pooled cohort. Notably, there was no evidence of effect modification by LVEF (all p for interaction >0.05), nor was there any attenuation of benefits in patients with LVEF >60 percent.9 (Figure)
Dapagliflozin may have the ability to reverse cardiac remodelling. The DAPA-MODA study showed that dapagliflozin was associated with improvements in LAVI (-6.6 percent; 95 percent CI, -11.1 to -1.8; p=0.008) and left ventricular mass index (LVMI; -13.9 percent; 95 percent CI, -18.7 to -8.7; p<0.001) as well as reductions in NT-proBNP level (-18.2 percent; 95 percent CI, -27.1 to -8.2; p<0.001) at 180 days in stable outpatients with chronic HF on optimized therapy.10
Reversed cardiac remodelling was also observed in our patient, as evidenced by reductions in left ventricular size and LAVI after 3 months of dapagliflozin treatment. Additionally, there was a decrease in GLS, a sensitive marker of myocardial dysfunction in HFpEF that strongly predicts clinical events and future deterioration in LVEF.11