Long-term single antiplatelet therapy for East Asian patients after PCI









Patients presenting with acute coronary syndrome (ACS) often require percutaneous coronary intervention (PCI) to restore cardiac function, and those with chronic coronary syndrome (CCS) may also be treated with PCI to improve clinical outcomes. After PCI, antiplatelet therapy is indicated to prevent future ischaemic events. However, it may increase the risk of bleeding. In an interview with MIMS Doctor, Dr Tat-Chi Leung, Specialist in Cardiology in Hong Kong, and Professor Hyo-Soo Kim from the Seoul National University College of Medicine, South Korea, discussed strategies to improve cardiovascular (CV) outcomes and reduce bleeding complications with antiplatelet therapy, particularly clopidogrel, in East Asian patients with ACS or CCS, including those in Hong Kong.
DAPT for ACS and CCS
Dual antiplatelet therapy (DAPT) with aspirin and an oral P2Y12 inhibitor, such as clopidogrel, ticagrelor or prasugrel, is the mainstay of antithrombotic therapy after myocardial infarction (MI) and/or PCI. [Eur Heart J 2023;44:3720-3826; Eur Heart J 2020;41:407-477]
The European Society of Cardiology (ESC) guidelines recommend DAPT for ≥12 months for patients with ACS, and for 6 months for CCS patients with increased risk of ischaemic events or after PCI. Nevertheless, the choice of P2Y12 inhibitor and the duration of DAPT can be adjusted when balancing between ischaemic and bleeding risks. [Eur Heart J 2023;44:3720- 3826; Eur Heart J 2020;41:407-477]
“Patients presenting with ACS often have higher risk of thrombotic events than those with CCS. As such, duration of DAPT is generally longer in ACS patients, but once their condition is stabilized, they should be changed to single antiplatelet therapy [SAPT] for maintenance,”Leung noted. [Rev Esp Cardiol (Engl Ed) 2022;75:360-363]
“In general, patients with high ischaemic risk relative to bleeding risk require a longer DAPT duration after PCI to prevent thrombotic events, whereas those with high bleeding risk [HBR] may need to shorten DAPT duration. The relative trade-off between the risk of ischaemia and bleeding will therefore determine the optimal DAPT duration,” said Leung. “Various clinical and procedural factors may influence ischaemic and bleeding risks, hence the DAPT duration. For instance, older age and comorbidities, such as diabetes, previous MI or heart failure, are clinical factors that increase both the risks of ischaemia and bleeding. Coronary factors, such as bifurcation diseases, poor systolic function, and complex PCI [eg, multiple vessels treated, multiple stents implanted, intervention on the left main coronary artery], also increase the risk of ischaemia and/or bleeding. We sometimes use the DAPT score to assess the benefit and risk ratio when determining the optimal duration of DAPT.” [Circ Cardiovasc Interv 2021;14:e009642; Catheter Cardiovasc Interv 2021;97:E758-E770; Front Cardiovasc Med 2022:8:729432; Catheter Cardiovasc Interv 2021;97:569-578]
Ethnic differences in ischaemic and bleeding risks
“Apart from individual factors, evidence suggests ethnic differences in bleeding risk in response to antiplatelet agents,” highlighted Leung. “East Asians, including patients in Hong Kong, tend to have higher bleeding risk and lower ischaemic risk than Caucasians.”
A landmark meta-analysis of seven randomized controlled trials (RCTs; n=16,518) that compared short- vs prolonged-duration DAPT after drug-eluting stent (DES) implantation revealed that East Asians had a two-fold lower rate of ischaemic events (hazard ratio [HR], 0.487; 95 percent confidence interval [CI], 0.341–0.697; p<0.001) and a two-fold higher rate of major bleeding events (HR, 2.262; 95 percent CI, 1.217–4.204; p=0.010) vs non-East Asians. Furthermore, prolonged DAPT was associated with increased risk of major bleeding in East Asians (HR, 2.843; 95 percent CI, 1.474–5.152; p=0.002) but not in non-East Asians (HR, 1.375; 95 percent CI, 0.523–3.616; p=0.523). A significantly greater proportion of East Asians had a higher probability of bleeding than ischaemia vs non-East Asians (32.3 vs 0.4 percent; p<0.001). [Thromb Haemost 2019;119:149-162]
“Nonetheless, about two-thirds of the East Asian patients still had a higher probability of ischaemia than bleeding. Therefore, we need to adjust antiplatelet therapy to effectively suppress thrombosis while minimizing the risk of bleeding complications in this population,” Kim remarked.
Strategies to mitigate bleeding risk in East Asians
Clopidogrel-based DAPT
Although DAPT with potent P2Y12 inhibitors (ticagrelor and prasugrel) showed superior antithrombic efficacy vs clopidogrel in the PLATO and TRITON trials, which predominantly enrolled Caucasians (≥91 percent), clopidogrel demonstrated comparable efficacy vs ticagrelor or prasugrel in studies conducted in East Asian patients (PHILO, KAMIR NIH, TICAKOREA, TALOS-AMI). Moreover, ticagrelor and prasugrel were associated with higher rates of bleeding than clopidogrel in all these studies, irrespective of ethnicity. [N Engl J Med 2009;361:1045-1057; N Engl J Med 2007;357:2001-2015; Circ J 2015;79:2452-2460; Thromb Haemost 2018;118:591-600; Circulation 2019;140:1865-1877; Lancet 2021;398:1305-1316]
“Ticagrelor or prasugrel may be too strong for East Asians, in terms of increased bleeding risk, and may not benefit them as much as Caucasians,” Kim noted. “Because of the bleeding risk associated with potent P2Y12 inhibitors, the majority of physicians in South Korea nowadays tend to treat post-PCI patients with clopidogrel-based DAPT. This trend is also reflected in the HOST-IDEA study, in which ≥88 percent of patients presenting with ACS or CCS were prescribed clopidogrel-based DAPT at physician’s discretion after PCI.” [Circulation 2023;147:1358-1368]
Shortened DAPT duration
“Years ago, ACS or post-PCI patients were routinely treated with DAPT for ≥12 months. However, evolving evidence suggests that shortened DAPT may be a safe option in East Asian patients. Clopidogrel-based DAPT is my preferred choice now, as it provides good thrombotic event protection with potentially reduced bleeding complications,” Leung commented. [Circulation 2023;147:1358-1368; Eur Heart J 2023;44:3720-3826]
“We usually shorten DAPT to 1–3 months followed by monotherapy in patients with HBR, low procedure complexity, simple lesions, low ischaemic risk, and low DAPT score,” Kim added.
DAPT de-escalation
The ESC guidelines stated that P2Y12 inhibitor de-escalation (switching from ticagrelor or prasugrel to clopidogrel) ≥30 days after the index ACS event may be considered to reduce the risk of bleeding events. For HBR cases, aspirin or P2Y12 inhibitor monotherapy after 1 month of DAPT may be considered. [Eur Heart J 2023;44:3720-3826; Lancet 2021;398:1305-1316]
“In Hong Kong, DAPT de-escalation is a common practice as many patients here generally have HBR,” Leung noted.
“In Korea, in case of recurrent bleeding, we may even step down to clopidogrel SAPT transiently to stabilize the bleeding and reassess the condition before deciding when to resume clopidogrel-based DAPT or whether to continue with clopidogrel monotherapy,” Kim added.
Long-term SAPT choice for East Asians
“Current guidelines recommend SAPT with aspirin, or P2Y12 inhibitors [eg, clopidogrel] as an alternative, after DAPT discontinuation as lifelong maintenance therapy regardless of the index clinical presentation,” pointed out Kim. “However, RCTs have demonstrated that monotherapy with clopidogrel is better than aspirin in reducing thrombosis as well as bleeding complications in the chronic maintenance phase following PCI.” [Eur Heart J 2023;44:3720-3826; Cardiology 2024;doi:10.1159/000537706]
HOST-EXAM trial: Clopidogrel superior to aspirin
In the HOST-EXAM trial (n=5,530), clopidogrel and low-dose aspirin were compared head-to-head as SAPT during the maintenance phase in Korean patients who received DES without clinical events for 6–18 months after PCI. During the 24-month follow-up, the primary outcome (a composite of all-cause death, nonfatal MI, stroke, readmission due to ACS, and major bleeding [Bleeding Academic Research Consortium (BARC) bleeding type ≥3]) occurred in significantly fewer patients receiving clopidogrel vs aspirin (5.7 vs 7.7 percent; HR, 0.73; 95 percent CI, 0.59–0.90; p=0.0035), with an absolute risk reduction of 2 percent (95 percent CI, 0.6–3.3). [Lancet 2021;397:2487-2496]
The secondary composite thrombotic endpoint (cardiac death, nonfatal MI, stroke, readmission due to ACS, or definite or probable stent thrombosis) also occurred in significantly fewer patients receiving clopidogrel vs aspirin (3.7 vs 5.5 percent; HR, 0.68; 95 percent CI, 0.52–0.87; p=0.0028). Additionally, fewer patients treated with clopidogrel vs aspirin had any bleeding (BARC type ≥2) (2.3 vs 3.3 percent; HR, 0.70; 95 percent CI, 0.51–0.98; p=0.036) and major bleeding (1.2 vs 2.0 percent; HR, 0.63; 95 percent CI, 0.41–0.97; p=0.035).
HOST-EXAM Extended trial: Long-term outcomes with clopidogrel
Long-term outcomes with clopidogrel and aspirin monotherapy were compared in the HOST-EXAM Extended trial, in which 4,717 patients from the HOST-EXAM trial were followed up for a median duration of 5.8 years after randomization for the same primary and secondary endpoints as in HOST-EXAM. “Clopidogrel was still superior to aspirin in both the primary [12.8 vs 16.9 percent; HR, 0.74; 95 percent CI, 0.63–0.86; p<0.001] and secondary thrombotic endpoints [8.1 vs 11.9 percent; HR, 0.66; 95 percent CI, 0.55–0.79; p<0.001], even with prolonged follow-up of nearly 6 years,” Kim remarked. [Circulation 2023;147:108-117]
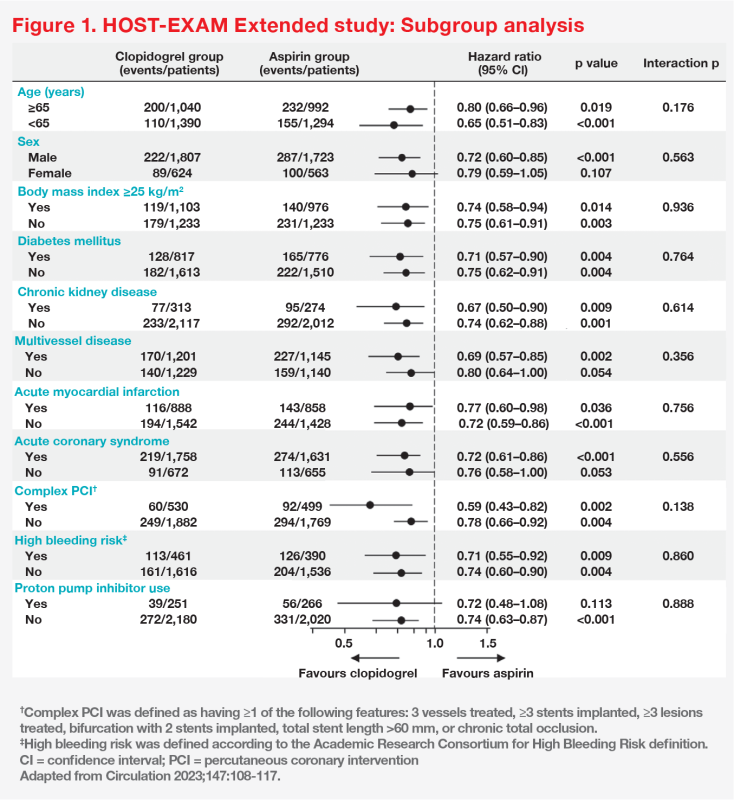
“Even though most patients [72 percent] presented with ACS at baseline, the beneficial effects of clopidogrel monotherapy were consistent in all patients throughout the extended follow-up period. This suggests that monotherapy with clopidogrel as chronic maintenance after PCI is better than aspirin irrespective of index clinical presentation,” Kim commented. “Importantly, the beneficial effect of clopidogrel vs aspirin monotherapy was also consistently shown across all high-risk subgroups, including patients with diabetes, chronic kidney disease, multivessel disease, and complex PCI, indicating a greater benefit with clopidogrel for patients with higher risk of thrombosis or recurrence.” (Figure 1)
Clopidogrel benefits patients with high thrombotic and bleeding risks
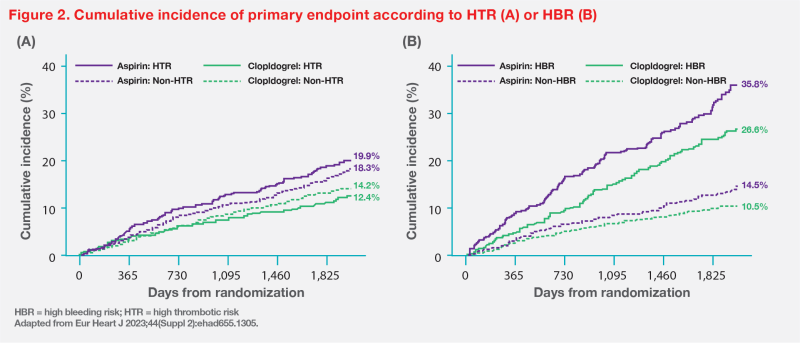
A post-hoc subgroup analysis of the HOST-EXAM Extended trial assessed the optimal SAPT during chronic maintenance phase in patients with high thrombotic risk (HTR) and/or HBR.
HTR was defined as patients with ≥1 of the following procedural features: 3 vessels treated, ≥3 stents implanted, ≥3 lesions treated, bifurcation with 2 stents implanted, total stent length >60 mm, or chronic total occlusion. HBR was defined according to the Academic Research Consortium for High Bleeding Risk (ARCHBR) criteria. The primary endpoint was a composite of all-cause death, nonfatal MI, stroke, readmission due to ACS, and BARC bleeding type 3 or 5. [Eur Heart J 2023;44:ehad655.1305]
Clopidogrel consistently reduced the risk of the primary endpoint vs aspirin regardless of presence or absence of HTR or HBR (with HTR: absolute risk difference [ARD], 7.5 percent; 95 percent CI, 2.7–12.3; HR, 0.59; 95 percent CI, 0.42–0.82; log-rank p=0.001) (without HTR: ARD, 4.1 percent; 95 percent CI, 1.5–6.7; HR, 0.78; 95 percent CI, 0.66–0.92; log-rank p=0.004) (with HBR: ARD, 9.2 percent; 95 percent CI, 2.4–16.0; HR, 0.71; 95 percent CI, 0.55–0.92; log-rank p=0.008) (without HBR: ARD, 4.0 percent; 95 percent CI, 1.6–6.4; HR, 0.74; 95 percent CI, 0.60–0.90; log-rank p=0.003). (Figure 2)
Bleeding risk: Clopidogrel vs aspirin
“The HOST-EXAM Extended trial also suggested that clopidogrel is better than aspirin in terms of grade and site of bleeding. Firstly, BARC type 3 bleeding was significantly more prevalent in the aspirin vs clopidogrel group [3.9 vs 2.6 percent; p=0.015]. Secondly, the aspirin group had higher rates of gastrointestinal [GI; 2.9 vs 2.2 percent], genitourinary [0.7 vs 0.4 percent] and intracranial bleeding [1.0 vs 0.5 percent] vs the clopidogrel group,” reported Kim. (Table)
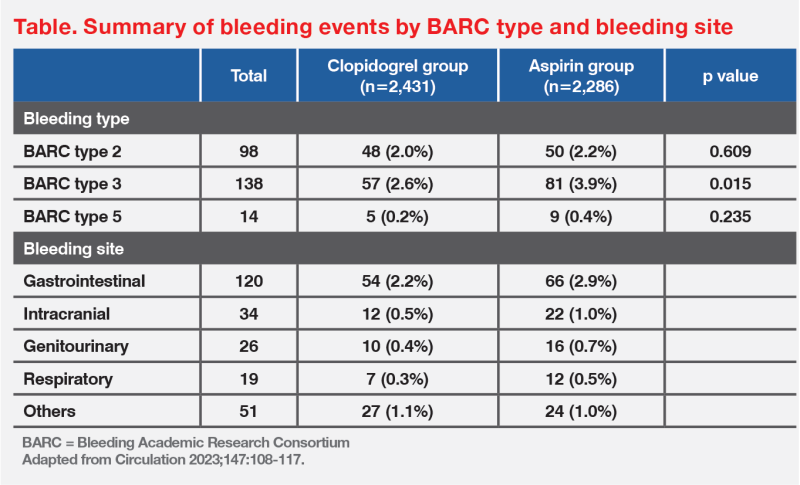
“Unlike clopidogrel, which prevents platelet aggregation through selectively inhibiting the platelet P2Y12 receptor, aspirin’s weaker antithrombotic effect is mediated via inhibition of prostaglandins and cyclooxygenase activity, which may also affect tissue integrity, thereby increasing the likelihood of GI and intracranial bleeding,” Kim explained. [Circulation 2023;147:108-117; Clopidogrel Hong Kong Prescribing Information, January 2021; Circulation 2000;101:1206-1218; Aliment Pharmacol Ther 2006;23:1225-1233; JAMA Netw Open 2023;6:e2325803]
Upper GI side effects (eg, dyspepsia) are common with low-dose aspirin. [J Gastroenterol 2015;50:626-637] “In our practice, clopidogrel would be a more suitable choice for patients who experience [upper] GI side effects,” said Leung.
Clinical considerations for using clopidogrel-based SAPT
“Lifelong SAPT is recommended in patients with ACS or CCS, especially after coronary stenting,” Kim said.
“However, clopidogrel SAPT should be temporarily discontinued 7 days before elective surgery and resumed after the surgery. Dehydration and excessive stress should be avoided, as they may increase platelet count and induce platelet activation, respectively,” Kim noted. “Based on anecdotal evidence, most surgeons believe aspirin, but not clopidogrel, can be continued during surgery. However, this needs to be confirmed by RCTs. Nevertheless, emergency surgery should not be a clinically significant concern for prescribing clopidogrel SAPT, because the need for emergency surgery is quite uncommon in practice.” [Blood 2016;127:1024-1035; Yeditepe Medical Journal 2015;9:875-883; Circulation 2023;147:108-117]
“Physicians should educate patients on the importance of drug compliance with antiplatelet therapy for preventing ischaemic events,” said Leung. “Antiplatelet therapy should not be discontinued prematurely without consulting physicians for minor bleeding, such as bruising.”
“Clopidogrel is the cornerstone antithrombotic agent for East Asian patients receiving PCI. Keeping other risk factors, such as blood glucose, blood pressure and LDL-cholesterol, under control is also paramount for improving CV outcomes,” Kim concluded.