Neoadjuvant PD-1 ICI plus chemotherapy in early-stage resectable NSCLC









Presentation, treatment and response
A 79-year-old male chronic drinker and smoker, with a 60 pack-years smoking history, presented with an incidental finding of a right middle lobe lung mass following a chest CT scan for aorta-related pathology in June 2023. He had hypertension, mild chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD) and abdominal aortic aneurysm (AAA) with known celiac and inferior mesenteric artery (IMA) stenosis.
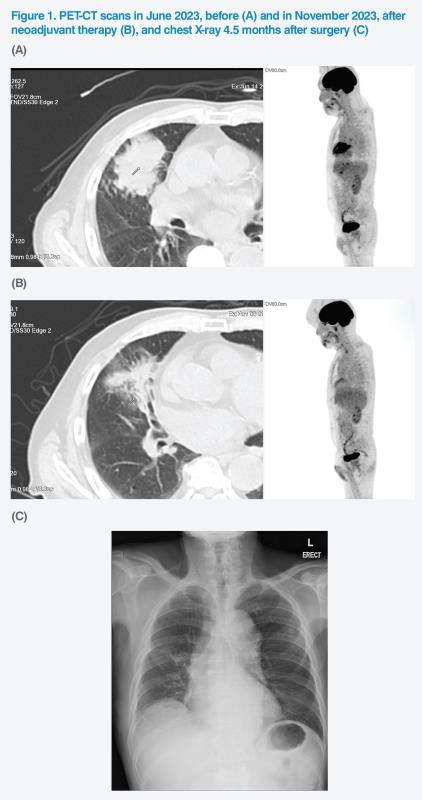
The hypermetabolic lung mass measured 7.3 x 6.8 cm and had a maximum standardized uptake value (SUVmax) of 15.9. (Figure 1A) The patient’s ipsilateral paratracheal, hilar and subcarinal lymph nodes (LNs) were hypermetabolic, suggesting stage III disease (stage IIIB, T4N2M0 disease based on the 8th edition of the AJCC staging criteria).1,2 CT-guided biopsy confirmed squamous-cell non-small-cell lung cancer (NSCLC). Molecular testing confirmed EGFR-negative disease with insufficient tissue for further ALK and PD-L1 expression level testing.
The patient was relatively fit, with a baseline Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 1. His disease was assessed to be resectable, and he was recommended neoadjuvant immunotherapy with nivolumab (intravenous [IV], 360 mg Q3W) plus paclitaxel and carboplatin to facilitate preoperative tumour shrinkage, which was commenced on 30 August 2023.1,3
The patient completed neoadjuvant therapy on 11 October 2023. He tolerated treatment well, with no dose reductions or treatment interruptions. Follow-up PET-CT scan showed substantial gross reduction of the lung mass to 7.0 x 3.5 cm. SUVmax declined to 4.3. (Figure 1B)
Surgery was performed on 24 November 2023. Dense adhesions around the right middle lobe (superior pulmonary vein area) were discovered intraoperatively, which resulted in moderate bleeding, necessitating conversion from minimally invasive surgery to open thoracotomy. Middle lobectomy of the right lung and right upper lobe anterior segmentectomy were performed, as the tumour crossed the fissure. The operation took 3.5 hours and was otherwise uneventful, with a total blood loss of 450 mL and no postoperative air leaks.
The patient experienced some postoperative complications, including chest infection, sepsis, atrial fibrillation, and COPD exacerbation. These were adequately managed and controlled with medications (ie, airway puffs with budesonide/formoterol, prednisolone, intravenous levoflaxacin, and amiodarone). He was discharged from hospital after 7 days.
Postoperative pathology report confirmed that the patient achieved pathological complete response (pCR). After discussing succeeding treatment options, the patient and his family decided to have no adjuvant therapy. The patient was last seen on 11 April 2024 and remained well. (Figure 1C) He will be regularly monitored for signs of disease progression.
Discussion
Neoadjuvant therapy is an important component of resectable NSCLC management, which is intended to facilitate subsequent surgery. Its successful implementation requires concerted efforts of a multidisciplinary team consisting of oncologists, surgeons, radiologists and molecular pathologists.1
From a surgical perspective, the goal of neoadjuvant immunotherapy in NSCLC management is to improve tumour resectability, treat any micrometastatic disease, and prime the patient’s immune system against recurrence while a large-volume tumour and tumour antigens are still present.1,4-6 Neoadjuvant therapy is not intended to convert unresectable tumours to resectable ones, and initial resectability is one of the key eligibility criteria for receiving neoadjuvant nivolumab.1,3,4
The open-label, randomized phase III CheckMate 816 trial in 358 patients with resectable NSCLC compared use of three neoadjuvant cycles of nivolumab plus platinum-doublet chemotherapy or chemotherapy alone, followed by resection. Patients with known EGFR mutations or ALK translocation were excluded.4
Patients in the nivolumab vs chemotherapy alone group had higher rates of minimally invasive surgery (30 vs 22 percent), lower rates of conversion from minimally invasive to open surgery (11 vs 16 percent), higher lobectomy rates (77 vs 61 percent), lower pneumonectomy rates (17 vs 25 percent), and higher R0 resection rates (83 vs 78 percent).7
Most patients in both treatment arms had surgery within the protocol-specified time window. No increase in median duration of surgery (184 vs 217 minutes) and length of hospitalization (10.0 vs 10.0 days) was found with the addition of nivolumab to neoadjuvant chemotherapy vs chemotherapy alone. Neoadjuvant nivolumab was not associated with an increased incidence of surgery-related AEs and did not impede the feasibility and timing of surgery, or the extent or completeness of resection vs chemotherapy alone.7
Although our patient required thoracotomy instead of minimally invasive surgery after intraoperative discovery of adhesions, it is difficult to ascertain whether those were the result of neoadjuvant treatment with nivolumab. In our clinical experience, surgery-complicating adhesions are strongly associated with neoadjuvant chemoradiotherapy, while neoadjuvant immunotherapy may not have the same effect.8
Of note, some patients who receive neoadjuvant ICI therapy may exhibit a phenomenon of “nodal immune flare”, which manifests as an unusual radiological appearance of LN enlargement. While this finding mimics disease progression, pathological evaluation may show increased immune cell infiltration and regression in cancer. Therefore, invasive pathological evaluation of LNs that are deemed suspicious by radiological criteria may be necessary for establishing or ruling out true progression.9
Since neoadjuvant chemotherapy offers minimal pCR rates and only improves 5-year recurrence-free survival and overall survival (OS) rates by approximately 5 percent vs surgery alone, neoadjuvant immunotherapy offers a much-needed alternative.8,10,11
Nivolumab (in combination with platinum-doublet chemotherapy) is the first immune checkpoint inhibitor (ICI) recommended for neoadjuvant treatment of patients with early-stage resectable NSCLC. On the basis of CheckMate 816 results, international guidelines recommend strong consideration of neoadjuvant nivolumab plus chemotherapy for patients with stage IB (≥4 cm) to IIIA NSCLC without EGFR or ALK aberrations.1,3,4
The addition of nivolumab to chemotherapy significantly improved the primary endpoint of pCR rate in the overall CheckMate 816 population, regardless of extent of resection (24.0 vs 2.2 percent; odds ratio, 13.94; 99 percent CI, 3.49–55.75; p<0.001). Importantly, this pCR benefit was observed across all key subgroups, irrespective of disease stage, tumour PD-L1 expression level and histologic type.4
The trial also achieved its other primary endpoint of EFS, which was longer with nivolumab plus chemotherapy vs chemotherapy alone.4 In the 4-year update from CheckMate 816, median EFS was 43.8 months with nivolumab plus chemotherapy vs 18.4 months with chemotherapy alone (hazard ratio [HR], 0.66; 95 percent confidence interval [CI], 0.49–0.90). The respective 48-month EFS rates were 49 and 38 percent.12
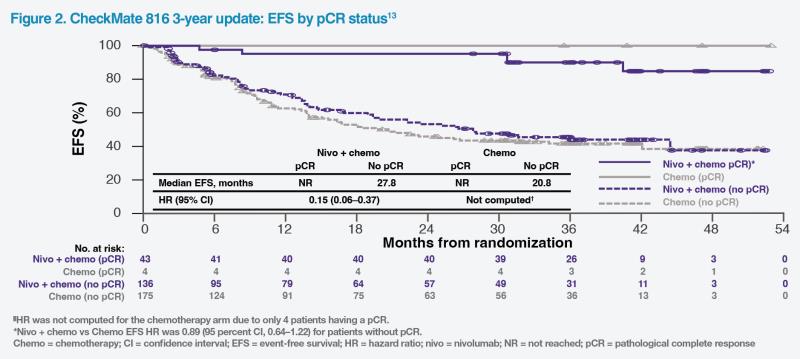
CheckMate 816 investigators noted the strong association between pCR and clinical benefit and suggested that pCR may be used as an early indicator of therapeutic efficacy in resectable NSCLC.4 In the 3-year update of CheckMate 816, among patients with a pCR, median event-free survival (EFS) was not reached in both treatment groups. In patients without a pCR, median EFS was 27.8 months in the nivolumab group vs 20.8 months with chemotherapy alone (HR, 0.89; 95 percent CI, 0.64–1.22). (Figure 2) Similar results were observed in terms of overall survival (OS). These results show that pCR was associated with both improved EFS and OS in patients treated with neoadjuvant nivolumab plus chemotherapy as well as those treated with chemotherapy alone.13
In the 4-year update from CheckMate 816, although median OS was not reached in either arm, neoadjuvant nivolumab plus chemotherapy demonstrated a clinically important OS improvement trend vs chemotherapy alone (HR, 0.71; 98.36 percent CI, 0.47–1.07; p=0.0451), which, however, did not meet significance boundary. The addition of nivolumab to chemotherapy improved lung cancer–specific survival vs chemotherapy alone (unstratified HR, 0.62; 95 percent CI, 0.41–0.93).12
In terms of overall safety, the incidence of grade 3/4 treatment-related AEs (TRAEs) was generally similar between the nivolumab plus chemotherapy and chemotherapy alone groups (33.5 and 36.9 percent). The most common grade 3/4 TRAEs were neutropenia (8.5 vs 11.9 percent) and decreased neutrophil count (7.4 vs 10.8 percent). Importantly, the incidence of immune-mediated AEs was low, and events were mainly of grade 1/2. The most common immune-mediated AE of any grade with nivolumab plus chemotherapy was rash (8.5 percent).4 The safety profile of neoadjuvant nivolumab plus chemotherapy remained consistent with previous reports in the latest 4-year update.12
Conclusion
The present case and results of the first positive phase III trial of immunotherapy-based combination neoadjuvant therapy support use of neoadjuvant nivolumab in combination with platinum-based chemotherapy in patients with early-stage resectable NSCLC and no actionable mutations.1,4,7,12